In our illuminative article titled “Understanding Immature Granulocytes: A Comprehensive Explanation,” we delve deep into the intricate world of immature granulocytes. With precise and factual information, we aim to provide a comprehensive overview of this intriguing subject. Found abundantly in the blood, these unique cells play a vital role in our immune system. By dissecting their formation, functions, and clinical implications, we hope to equip our readers with a thorough understanding of immature granulocytes and shed light on their significance in maintaining optimal health.

Definition and Overview
What are granulocytes?
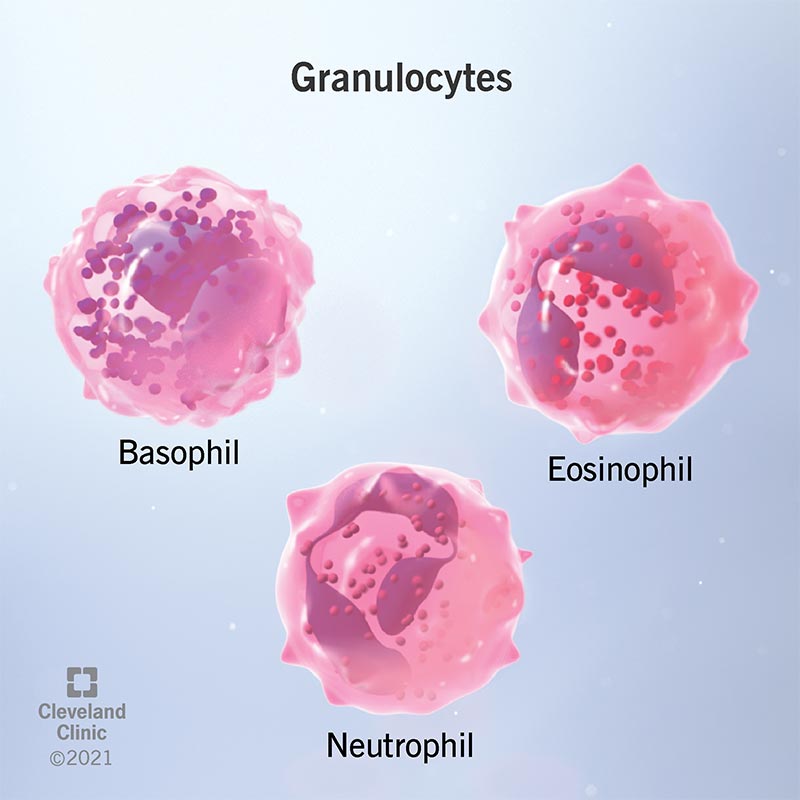
Granulocytes are a type of white blood cell, also known as leukocytes, that play a crucial role in the immune system. They are characterized by the presence of cytoplasmic granules in their cell bodies, which contain various substances that aid in their immune functions. Granulocytes are involved in the body’s defense against bacterial and fungal infections and are an essential component of the innate immune response.
What are immature granulocytes?
Immature granulocytes, also known as band or metamyelocytes, are a subset of granulocytes that are released into the bloodstream from the bone marrow during certain conditions. These cells are in the process of maturation and are considered to be intermediary between the immature myeloblasts and the fully matured granulocytes. The presence of immature granulocytes in the peripheral blood is often an indication of an underlying inflammatory or infectious process.
Types of immature granulocytes
There are three main types of immature granulocytes: myeloblasts, promyelocytes, and metamyelocytes. Myeloblasts are the earliest precursor cells of granulocytes in the bone marrow, while promyelocytes and metamyelocytes are more mature forms. These cells gradually develop and differentiate into fully mature granulocytes, such as neutrophils, eosinophils, and basophils.
Functions of immature granulocytes
Immature granulocytes are actively involved in the immune response against infections and inflammation. They have the ability to ingest and destroy pathogens, produce inflammatory mediators, and recruit other immune cells to the site of infection. Additionally, these cells play a key role in tissue repair and wound healing processes. By monitoring the presence and function of immature granulocytes, healthcare professionals can gain valuable insights into the body’s immune status and overall health.
Detection and Measurement
Laboratory testing methods
The detection and measurement of immature granulocytes can be performed through various laboratory testing methods. Manual differentials, performed by trained laboratory personnel, involve examining a blood smear under a microscope to identify and quantify the different types of white blood cells present. Automated hematology analyzers, on the other hand, use flow cytometry technologies to analyze blood samples and provide automated differential counts, including the levels of immature granulocytes.
Normal range of immature granulocytes
The normal range of immature granulocytes in the peripheral blood varies depending on several factors, including age and underlying health conditions. Generally, healthy individuals have low levels of immature granulocytes, usually less than 5%. However, certain physiological conditions, such as pregnancy or intense physical exercise, can transiently elevate the levels of these cells. It is important to compare the measured levels with appropriate reference ranges to accurately interpret the results.
Clinical significance of elevated immature granulocytes
Elevated levels of immature granulocytes, known as a left shift, are often indicative of an ongoing immune response, such as infection or inflammation. In such cases, the bone marrow releases immature granulocytes into the bloodstream to compensate for the increased demand for these cells. Monitoring the levels of immature granulocytes can help healthcare professionals assess the severity and progression of infections, evaluate the response to treatment, and predict the prognosis and outcomes of certain conditions.

Causes of Increased Immature Granulocytes
Infection and inflammation
Infections, both bacterial and fungal, as well as inflammatory conditions, can trigger the release of immature granulocytes from the bone marrow. This response is part of the body’s defense mechanism to combat the invading pathogens and initiate the inflammatory process. Conditions such as pneumonia, urinary tract infections, and appendicitis may lead to increased levels of immature granulocytes in the peripheral blood.
Bone marrow disorders
Certain bone marrow disorders can disrupt the normal maturation process of granulocytes, resulting in the accumulation of immature cells in the bloodstream. Conditions such as acute myeloid leukemia (AML), myelodysplastic syndrome (MDS), and myeloproliferative neoplasms (MPNs) can cause a significant increase in the levels of immature granulocytes. In these cases, further investigation and diagnostic tests are necessary to determine the underlying cause and develop an appropriate treatment plan.
Medication-related factors
Certain medications, particularly those that stimulate the production of white blood cells, can lead to an increase in immature granulocytes. Drugs such as corticosteroids, granulocyte colony-stimulating factors (G-CSFs), and certain chemotherapeutic agents may cause a left shift by promoting the release of immature granulocytes from the bone marrow. Healthcare professionals should consider medication history when interpreting the results of immature granulocyte measurements.
Stress and physiological conditions
Stress and physiological conditions, such as strenuous exercise, pregnancy, and certain chronic diseases, can temporarily elevate the levels of immature granulocytes. The stress response triggers the release of cortisol, a hormone that influences the production and release of white blood cells from the bone marrow. These transient increases in immature granulocytes should be interpreted in conjunction with clinical symptoms and other laboratory findings to determine their significance.
Diagnostic Applications
Impact on diagnosing infections
The presence of elevated immature granulocytes can provide valuable diagnostic information in the context of infections. In cases where the exact source of infection is unclear, increased levels of immature granulocytes can indicate the presence of a bacterial or fungal infection. Furthermore, the serial monitoring of immature granulocyte levels throughout the course of treatment can help assess the effectiveness of antimicrobial therapy and guide clinical decision-making.
Differentiating between acute and chronic conditions
Evaluating the levels of immature granulocytes can assist in distinguishing between acute and chronic conditions. In acute infections or inflammatory processes, a temporary increase in immature granulocytes may be observed. Conversely, chronic conditions associated with ongoing inflammation or infections, such as autoimmune disorders or chronic granulomatous diseases, may exhibit persistently elevated levels of immature granulocytes. These findings can aid in the differentiation and management of various medical conditions.
Monitoring therapeutic responses
Monitoring immature granulocyte levels can be useful in assessing the response to treatment. A decrease in the levels of immature granulocytes over time may indicate that the therapy is effectively addressing the underlying infection or inflammatory condition. Conversely, persistent or increasing levels of these cells may suggest treatment failure or the presence of a new infection. Regular monitoring and appropriate clinical correlation are essential to ensure appropriate management and adjustment of treatment plans.
Predicting prognosis and outcomes
Studies have shown that elevated levels of immature granulocytes are associated with poor prognosis and worse clinical outcomes in certain conditions, including cancer, sepsis, and autoimmune disorders. In cancer patients, the presence of increased immature granulocytes may indicate aggressive disease progression or resistance to therapy. Similarly, in sepsis, high levels of these cells have been linked to higher mortality rates. The predictive value of immature granulocytes can help clinicians stratify patients and develop individualized treatment plans.

Clinical Implications
Association with specific diseases
Elevated levels of immature granulocytes have been observed in various diseases and medical conditions. In acute bacterial infections, such as urinary tract infections or pneumonia, high levels of immature granulocytes may suggest a localized site of infection. In chronic inflammatory conditions, such as rheumatoid arthritis or inflammatory bowel disease, persistently elevated levels of these cells may reflect disease activity. Identifying the underlying cause of the increase in immature granulocytes is crucial in managing these diseases effectively.
Prognostic significance in cancer patients
The presence of increased immature granulocytes has been identified as an adverse prognostic factor in multiple types of cancer. A high proportion of immature granulocytes, particularly in patients with solid tumors or hematological malignancies, is associated with advanced disease stage, lower survival rates, and resistance to therapy. Clinicians can utilize these findings to identify high-risk patients and optimize treatment strategies accordingly for improved patient outcomes.
Risk assessment in sepsis
Sepsis is a life-threatening condition characterized by a dysregulated immune response to infection. The early identification and risk stratification of septic patients are crucial for timely intervention and improved outcomes. Elevated levels of immature granulocytes have been shown to be an independent risk factor for increased morbidity and mortality in sepsis. Monitoring these levels can aid in the early identification of high-risk patients and guide appropriate treatment decisions.
Usefulness in monitoring autoimmune disorders
Autoimmune disorders, such as lupus or vasculitis, involve abnormal immune responses against the body’s own tissues. The measurement of immature granulocytes can provide insights into disease activity and treatment response in these conditions. Persistent elevation of immature granulocytes may indicate ongoing inflammation and autoimmune activity, while a decline in these cells can signify improvement in disease control. Regular monitoring of immature granulocyte levels can guide the management of autoimmune disorders and help optimize treatment approaches.
Interpretation Challenges
Interfering factors in measurement
Several factors can influence the measurement and interpretation of immature granulocytes. Pre-analytical factors, such as improper sample handling or storage, may affect the integrity of the cells and lead to inaccurate results. Additionally, medications, such as G-CSFs or corticosteroids, can impact the levels of immature granulocytes and should be taken into consideration when interpreting the results. It is essential to standardize and control these factors to ensure reliable and accurate measurements.
Differentiating between immature and mature granulocytes
Distinguishing between immature and mature granulocytes can be challenging, as their morphological and functional characteristics overlap. Manual differentials performed by skilled laboratory personnel help identify and classify these cells accurately, but there is still a degree of subjectivity involved in the process. Automated hematology analyzers are increasingly used to provide more objective and reproducible measurements, but further research and validation are needed to improve their accuracy in distinguishing between immature and mature granulocytes.
Importance of correlation with clinical symptoms
While the measurement of immature granulocytes provides valuable diagnostic information, it must be interpreted in conjunction with clinical symptoms and other laboratory findings. Elevated levels of immature granulocytes alone do not indicate a specific diagnosis or disease, but rather serve as a marker of an underlying immune response. Clinical correlation is essential to determine the significance of these findings and guide appropriate management decisions.
Treatment Considerations
Addressing underlying causes
When abnormal levels of immature granulocytes are detected, the underlying cause should be identified and addressed. In the case of infections, appropriate antimicrobial therapy is crucial for eliminating the pathogens and resolving the immune response. Treating underlying inflammatory or autoimmune conditions with immunosuppressive agents or disease-modifying medications may help reduce elevated levels of immature granulocytes. Targeted therapies, such as chemotherapy or stem cell transplantation, may be necessary in cases of bone marrow disorders.
Optimizing antibiotics and anti-inflammatory therapies
In the management of infections or inflammatory conditions associated with elevated immature granulocytes, selecting the appropriate antibiotics or anti-inflammatory therapies is critical. Identifying the specific pathogens through culture and sensitivity testing can guide the choice of antimicrobial agents. Additionally, anti-inflammatory medications, such as corticosteroids or nonsteroidal anti-inflammatory drugs (NSAIDs), can help alleviate the inflammatory response and reduce the release of immature granulocytes.
Supportive care strategies
Supportive care strategies play a crucial role in the management of conditions associated with elevated immature granulocytes. Adequate hydration, nutrition, and rest are essential for supporting the body’s immune system and promoting recovery. In severe cases, hospitalization and intensive care may be required to provide close monitoring and supportive therapies, such as intravenous fluids or oxygen supplementation.
Monitoring response to treatment
Regular monitoring of immature granulocyte levels is essential to assess the response to treatment and guide adjustments in therapeutic strategies. A decline in immature granulocytes indicates a favorable response to treatment, while persistent or increasing levels suggest treatment failure or the need for further interventions. Serial measurements, along with clinical evaluation and other laboratory tests, should be used to monitor the progress of the underlying condition and guide the duration and intensity of treatment.
Prognosis and Outlook
Predictive value for patient outcomes
The measurement of immature granulocytes has demonstrated predictive value for patient outcomes in various medical conditions. In cancer patients, high levels of immature granulocytes are associated with decreased survival rates and poorer treatment responses. Similarly, in sepsis, elevated levels of these cells have been linked to higher morbidity and mortality. Monitoring immature granulocytes can help identify patients at higher risk and guide treatment decisions to improve outcomes and overall prognosis.
Long-term effects on health
The long-term effects of elevated immature granulocytes on overall health are not yet fully understood. Persistent elevation of these cells, especially in the absence of an underlying infection or inflammation, may suggest an underlying bone marrow disorder. In such cases, comprehensive diagnostic evaluations are necessary to determine the exact cause and initiate appropriate treatment. Long-term follow-up and close monitoring are essential to evaluate the response to therapy and minimize potential health risks.
Prognostic implications in specific conditions
In specific medical conditions, the levels of immature granulocytes have prognostic implications. For example, in patients with acute myeloid leukemia (AML), a high proportion of immature granulocytes is associated with worse outcomes and decreased responses to chemotherapy. Similarly, in septic patients, elevated levels of immature granulocytes are indicators of increased morbidity and mortality. Understanding the prognostic implications of immature granulocytes can guide clinicians in prognosticating and managing these conditions more effectively.
Research and Future Directions
Advancements in measuring immature granulocytes
Advancements in laboratory techniques and technologies continue to improve the measurement of immature granulocytes. Automated hematology analyzers equipped with advanced flow cytometry capabilities offer increased accuracy and reproducibility in identifying and quantifying these cells. Ongoing research focuses on establishing standardized reference ranges and improving the sensitivity and specificity of these measurements. Additionally, the integration of artificial intelligence algorithms may facilitate the identification and classification of immature granulocytes, further enhancing diagnostic capabilities.
Exploring the role of immature granulocytes in immune responses
The role of immature granulocytes in immune responses is an area of ongoing research. Studies aim to elucidate the specific functions and mechanisms of action of these cells, particularly in the context of infection and inflammation. By understanding the role of immature granulocytes in the immune system, researchers and healthcare professionals can develop targeted therapies or interventions to modulate their function and optimize immune responses in various clinical settings.
Potential therapeutic targeting of immature granulocytes
Targeting immature granulocytes therapeutically is an emerging area of research. As these cells play a crucial role in the immune response, modulating their activity may offer potential therapeutic benefits. Manipulating the release, maturation, or function of immature granulocytes through pharmacological interventions or gene therapies may enhance the body’s immune response or mitigate inflammation in certain diseases. Comprehensive preclinical and clinical studies are necessary to evaluate the safety and efficacy of these interventions.
Identifying novel biomarkers for disease diagnosis and prognosis
While immature granulocytes provide valuable diagnostic and prognostic information, the search for additional biomarkers continues. Identifying novel biomarkers that complement the measurement of immature granulocytes may improve diagnostic accuracy and prognostic stratification in specific diseases. Biomarkers such as cytokines, chemokines, or genetic markers may help further refine the assessment of disease activity, treatment response, and prognosis. Research efforts in this field are focused on identifying and validating these potential biomarkers.
Conclusion
Understanding immature granulocytes and their clinical significance is crucial in the evaluation and management of various diseases and conditions. These cells serve as important indicators of the immune system’s response to infection, inflammation, and underlying physiologic changes. Monitoring the levels of immature granulocytes can aid in diagnosing infections, assessing treatment responses, predicting prognosis, and guiding therapeutic decisions. Ongoing research and advancements in laboratory techniques and biomarkers continue to enhance the understanding of immature granulocytes and their potential applications in clinical practice. By harnessing this knowledge, healthcare professionals can provide better patient care and improve outcomes in a wide range of medical conditions.